
Outreach is still the most effective way of reaching the 257 million people around the world who don’t have access to contraception. MSI Zambia shares their fresh approach to reaching people with life-changing reproductive choice — with outstanding results.
My beautiful home of Zambia is a vast and diverse landscape, with rugged rural regions where many communities live with limited access to what you and I take for granted, like contraception. Women who want contraception often don’t have access to health facilities and there’s often no one trained to provide services.
So our MSI Zambia outreach teams travel into the world’s most rural and remote communities with the highest unmet need for contraception. When our teams arrive, we offer them a range of contraceptive methods and a different future path — one that they choose.
Our outreach work complements the continuing efforts of Ministries of Health to expand healthcare as far as possible and our health system strengthening approach, so no one falls through the gap.
We’ve recently changed how we’re doing outreach, and the results speak volumes. In my 12 years of experience in the global health sector, I haven’t seen a better or more cost-effective way to reach rural communities and adolescents with contraceptive choice.
With our previous model, our outreach teams couldn’t go far enough to reach everybody — with each team only reaching 20 community sites every month. With our limited resources we knew we had to reassess, refine, and innovate.
We asked ourselves the million-dollar question: How can we reach more people in the most efficient way possible?
Here’s what we decided to do:
We split our teams in two and joined forces with the government
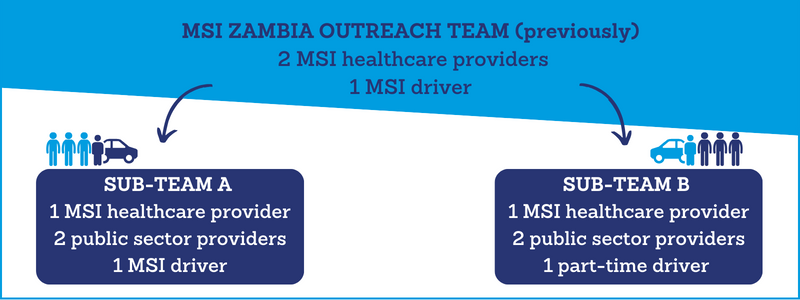
Previously, an MSI Zambia outreach team was made up of two healthcare providers and one driver. One week they’d travel to very rural places, and the next they would serve urban communities.
One team has now been divided into two sub-teams. We’ve contracted four healthcare providers from the Ministry of Health, and another part-time driver, so a single team can be in two places at once.
While one sub-team camps in rural places more than 100km from ‘basecamp’ to reach the furthest communities, the other is delivering urban-based services (when the urban-based team knock off at the end of the day, they go home to their families). They swap each week. To mobilise clients, we call the outreach sites the month before so they can let people in their area know which day we’re coming. When we get to a community site in the morning, it’s not uncommon to find 100 women lined up for contraception.
Clearly, we needed more than one healthcare provider to serve an entire community, so to bolster the outreach teams we partnered with the public sector. Two public healthcare providers are now integrated into each sub-team, mentored by the MSI provider. And we work closely with local providers when we visit their facilities.
So we now have more healthcare providers, a robust government partnership, and a far wider reach — extending out to people with the greatest need of contraceptive choice. The number of people each team can serve every month is now 4,700 — a 420% growth from when we used the old model just a few years ago.
It’s transformed how we do outreach forever.
I travel often with our outreach teams and see first-hand their daily embodiment of MSI’s commitment to quality healthcare. Some of our clients tell me how they walk tens of kilometres to get there; some pass through game parks, risking their lives against the likes of lions and elephants. These women can sometimes be desperate to use contraception, saying they can’t afford to look after the children they already have. In these moments, this is no longer ‘a job’. Without us, these women wouldn’t have a choice, wouldn’t have a chance. We are here to save their lives in every sense.
Ripple effect of building public provider skills
64 public sector healthcare providers are now fully integrated into our outreach teams for rolling six-month periods. Their immersion into MSI’s programme, under the expert guidance of MSI’s providers, builds their skills in delivering comprehensive and high-quality reproductive healthcare.
They learn how to deliver services confidently, independently, and efficiently — and broaden their knowledge on providing long-term and permanent contraceptive methods. This doesn’t end here. When they return to their public sector facilities, they bring skills back with them to teach others. And people receiving a service from them will benefit no matter where they go.
In return, these providers bring insights from the public health system and enable us to tap into their neighbourhood community networks, so we can mutually grow and reach more people.
Our credibility and relationships within the Ministry of Health have never been stronger. With partnerships like these, the impact we can have on women’s lives is exponentially greater.
Giving people long-term contraceptive options for the first time
Our outreach overhaul is about more than just numbers. We want to give people real contraceptive choice — short-term, long-term and permanent methods.
Many people in remote communities have never been able to access long-term methods which would help them avoid unintended pregnancy for longer. So our teams focus on delivering choices and clearly communicating options. We’ve seen a rise in clients seeking long-acting and permanent methods, from 71% with the previous outreach model to 94% with our new model.
For a woman who usually has to travel many kilometres to get her hands on a short-term method of contraception — when we turn up to her community offering a method like an IUD which will protect her for up to ten years, we change the course and quality of her life. Behind each method and every number is a woman’s future and I try not to lose sight of that.
MSI Zambia has been using this accelerated service delivery (split-teams) model since 2018, and the results are stark. We’re more efficient, helping more adolescents, supporting more people with long-term contraception methods — all while retaining exceptional clinical quality.
Most importantly, we’re reaching more people who may have had little or no prior access to life-changing reproductive choice.
This is a paradigm shift in reproductive health outreach. I’m incredibly proud to share our new gold-standard outreach model with other MSI country teams and the entire reproductive healthcare sector. Together, with continued investment and partnerships, we can set a new global benchmark and change countless lives.








